Request Appointment
New Patient - Priority Scheduling
Please fill out the form below, including all the required fields, and receive priority new patient scheduling.
If you’re living with low back pain, you’re definitely not alone. It’s one of the most common reasons people come to see us at Transform Chiropractic in Toronto.
For many, it starts as a dull ache after sitting too long or doing chores. Over time, it can turn into sharp pain with bending, stiffness in the morning, or even discomfort that shoots down into your hip or leg.
Most people try to manage it on their own at first. They stretch more, change their chair, buy a new mattress, or search YouTube for “best low back exercises.”
Sometimes those things help a little—but the pain keeps coming back, or never fully resolves. That can be frustrating and a bit worrying, especially when it starts affecting sleep, work, or family activities.
Here’s the good news: in most cases, low back pain is usually mechanical and postural in nature, which means there’s almost always a clear reason for it—and a structured way to correct it.
At Transform Chiropractic, we focus on understanding why your back is hurting in the first place. Through a detailed history, specific movement and orthopedic testing, and, when needed, digital spinal x-rays, we identify what’s really going on with your spine and nervous system.
From there, we create a personalized plan that combines gentle, precise chiropractic adjustments, soft tissue work, and simple at-home strategies to help restore motion and stability—so you can get back to the things you enjoy.
In this guide, you’ll learn what typically causes low back pain, how we assess it, and how chiropractic care can help you move and feel better—safely and naturally.
Your low back does a lot of work. It supports your upper body, allows you to bend and twist, and forms the foundation for your ribs and pelvis. When everything moves well, your joints, discs, and muscles share the load evenly. But when one area stiffens or weakens, others have to compensate and work overtime – that’s when irritation can begin.
The low back (lumbar spine) is built for both strength and movement. Five stacked vertebrae, flexible discs between each bone, facet joints that guide movement, and layers of stabilizing muscles and ligaments all work together to let you walk, lift, and sit comfortably—as long as forces are distributed evenly.
Modern life isn’t always kind to your low back. Long hours of sitting, repetitive bending and lifting, past injuries, or bad posture can gradually shift how your spine moves and where the stress goes. Over time, this can lead to:
• Joints that become stiff or restricted
• Discs that are placed under uneven pressure
• Muscles that are overworked in some areas and weak in others
• Irritation of nearby nerves
The result? Pain, stiffness, and that sense your back “just isn’t right.”
The key point: low back pain rarely comes out of nowhere. There is almost always a pattern underneath it—and once we understand that pattern, we can create a precise plan to correct it and to keep it from coming back.
Most low back pain doesn’t start with a single lift or one “wrong move.” It usually develops slowly, as your spine and supporting muscles adapt to the way you sit, stand, bend, and move every day.
Over time, a few predictable changes tend to occur:
Certain joints become stiff or “stuck.”
Other areas have to move more to make up for it, which increases wear and tear.
Muscles tighten and weaken in predictable patterns.
Hip flexors, hamstrings, or low-back muscles may tighten, while deep core and glute muscles gradually switch off.
Discs are loaded unevenly.
Repeated bending, sitting, or twisting in one direction can overload specific segments.
Ligaments slowly deform (“ligament creep”).
Holding one posture for hours each day allows the supporting ligaments to stretch and adapt to that stressed position.
Eventually, your body reaches a point where it can no longer compensate smoothly — and what started as a subtle imbalance finally shows up as pain, stiffness, or a sudden flare-up.
The encouraging part?
Because these patterns are mechanical and structural, they can usually be improved with the right combination of chiropractic care, movement, and simple daily changes.
Low back pain can come from many different sources. Some are simple muscle strains; others involve deeper spinal or nerve irritation. That’s why a proper assessment matters—two people can describe the same pain, yet the underlying cause can be very different.
Most people’s pain starts here:
• Muscle and ligament strain from lifting, twisting, or sitting too long.
• Joint irritation in the small facet joints at the back of the spine, often causing sharp, localized pain that can spread into the buttock or hip.
• Postural stress, especially from hours at a desk or leaning forward, which gradually overloads the spine and surrounding muscles.
These problems are very common and usually respond well to conservative chiropractic care and better movement habits.
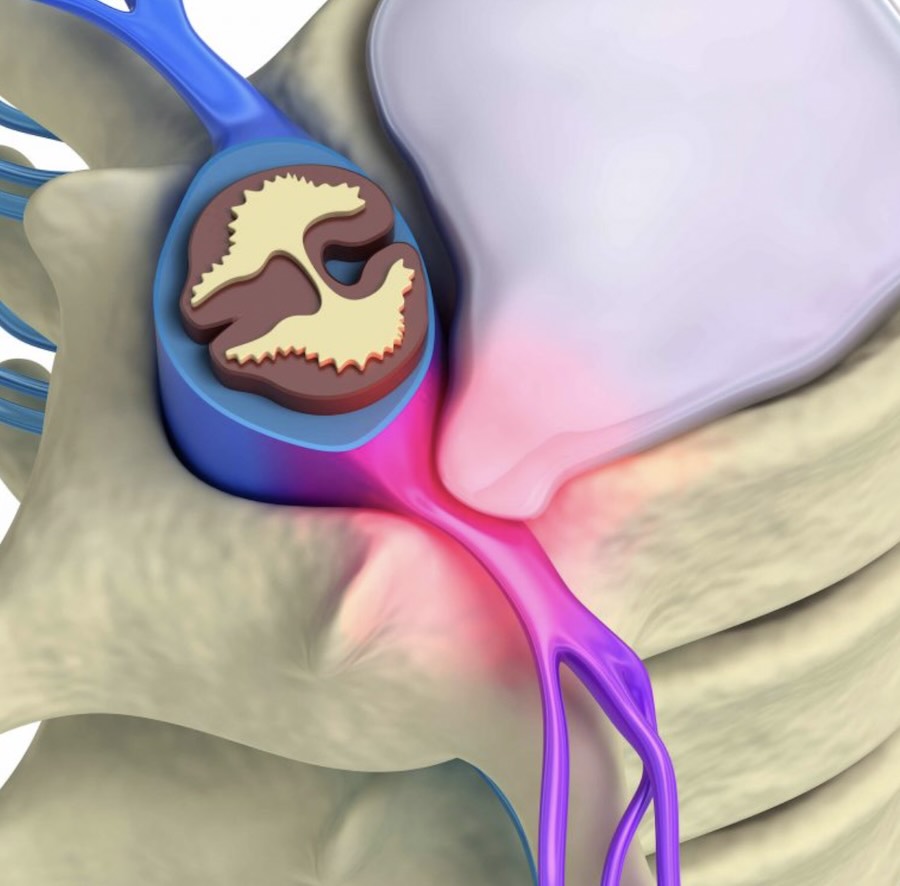
The discs between your vertebrae can sometimes bulge or shift, placing pressure on nearby nerves. When that happens, pain may travel down your leg—often called sciatica—and may include tingling or weakness.
Most disc-related problems don’t require surgery and can improve with careful, staged chiropractic treatment that reduces pressure and restores movement.
As we get older, natural changes such as disc height loss, mild arthritis, or spinal narrowing (stenosis) can make the back more sensitive to strain. Others may have minor spinal shifts or curves that change how forces travel through the joints.
Even with these long-standing patterns, gentle chiropractic care, postural work, and focused exercise can often reduce stiffness and improve comfort.
Not all low back pain behaves the same way. Understanding which pattern you’re dealing with helps us choose the safest, most effective treatment plan.
The most common type.
Pain is usually local to the low back or buttock, often worse with certain movements or positions and better with others. Often related to joint restriction, muscle strain, or postural overload.
Facet joints are the small joints at the back of the spine.
When irritated, they can cause sharp, localized pain, especially with extension (arching) or twisting, and may refer into the buttock or hip.
Disc-related pain often feels deeper and more diffuse.
It may worsen with bending, sitting, or lifting, and can sometimes send pain into the hip or leg.
When a spinal nerve becomes irritated or compressed, pain may travel down the leg.
Typical symptoms include sharp or burning pain, numbness, tingling, or weakness following a nerve pathway.
The joints where your spine meets your pelvis can become irritated or restricted.
This often causes pain off to one side, near the dimple at the back of the pelvis, sometimes radiating into the buttock or thigh.
Narrowing of the spinal canal or joint degeneration can make the back more sensitive to compression and standing.
People with stenosis often feel better when leaning forward or sitting, and worse with prolonged walking.
Tight, overworked muscles and trigger points can refer pain into the low back, hips, or even the legs.
This often co-exists with joint or disc issues and responds well when the underlying mechanics are corrected.
Part of your initial assessment is determining which of these patterns is most involved — so we can match your care to your actual condition rather than guessing.
Before recommending care, we start by understanding exactly what’s driving your pain. Guessing leads to frustration; clarity speeds recovery and leads to better results.
Your visit begins with a detailed conversation about your history—when the pain started, what makes it better or worse, and how it affects your work, sleep, and daily life.
Next, we look at posture, flexibility, and movement through the spine, hips, and pelvis. Gentle orthopedic and neurological tests help pinpoint which joints, muscles, or nerves are involved.
In some cases—especially with long-standing pain, previous trauma, or suspected structural changes—we may recommend digital spinal x-rays. These help us:
• See the alignment and curves of your spine
• Assess disc spaces and arthritic changes
• Identify areas of increased stress or instability
If we suspect a more serious disc or nerve issue that requires advanced imaging, we’ll coordinate with your medical doctor for MRI or specialist referral as needed.
The goal: a clear, personalized understanding of what’s happening—so your care can be specific, safe, and effective.

While almost anyone can develop low back pain, some groups are especially prone:
Desk workers and computer users
Long periods of sitting and flexed posture gradually overload the discs and joints.
Manual workers and tradespeople
Repetitive lifting, bending, twisting, and vibration all increase spinal stress.
Drivers and commuters
Sustained sitting combined with whole-body vibration makes the low back work harder.
Parents of young children
Frequent lifting, carrying, and awkward positions can strain the spine.
Athletes and active individuals
High loads, one-sided sports, and incomplete recovery can all contribute to recurring pain.
Older adults
Natural age-related changes (like disc thinning and arthritis) make the spine more sensitive to poor mechanics.
Knowing your risk profile helps us tailor both treatment and prevention strategies for your specific lifestyle.
Once we understand your unique pattern, we can build a treatment plan that fits your body—not a generic protocol.
Our approach focuses on safe, non-surgical back pain treatment options designed to restore movement and reduce discomfort naturally – without relying on invasive procedures.
Chiropractic adjustments are designed to improve the motion and alignment of the joints in your spine. When joints move better:
• Irritation on surrounding tissues is reduced
• Muscles can relax and rebalance
• Pressure on nearby nerves often decreases
At Transform Chiropractic, adjustments are tailored to your comfort level and structure. We use a range of techniques—from hands-on adjustments to lighter instrument-assisted methods—depending on what is most appropriate for you.
Muscles and fascia often adapt to protect irritated joints and discs. As part of your plan, we may use:
• Targeted soft tissue techniques to release tight or overworked muscles
• Gentle stretching and mobility work
• Guidance on when to use ice or heat at home
This combination helps reduce muscle tension and allows adjustments to hold more effectively.
For some patients—especially those with disc issues, postural collapse, or long-standing structural change—we may incorporate specific spinal traction or curve-supporting devices. These are always based on your assessment and imaging and are introduced gradually.
The goal is to gently unload irritated structures, improve alignment, and support healthier long-term mechanics.
Throughout your care, we’ll explain what we’re doing and why it matters:
• How to move and position your back during daily activities
• Which movements to temporarily avoid—and which to reintroduce
• How to pace your return to work, exercise, or hobbies
When you know what’s happening and what to expect, it’s easier to stay consistent and confident as you improve.
Hands-on care is only part of the solution. The other part is helping your muscles and nervous system support your spine between visits.
Depending on your assessment, we may recommend a small number of targeted exercises, such as:
• Bird-dog variations (cross-crawl) to activate deep core stabilizers
• Glute bridge progressions to strengthen your hips and protect your low back
• Side plank variations to build lateral stability
We’ll show you how to perform these correctly and adjust them to your current ability level. Often it’s better to do a few well-chosen exercises consistently than a long list done occasionally.

Gentle mobility work can help reduce stiffness and improve comfort, especially after periods of sitting or first thing in the morning. Examples include:
• Controlled cat-camel movements for segmental spinal mobility
• Simple hip and hamstring stretches, when appropriate
• Breathing and relaxation strategies to reduce protective muscle tension
These are introduced at the right time in your recovery—not too early, and not all at once.
Small daily changes can make a big difference:
• Breaking up long periods of sitting with brief standing or walking breaks
• Adjusting desk or workstation height
• Using supported positions for reading or screen time
• Building in gentle walking as tolerated
We’ll help you prioritize what matters most for your particular situation, so the plan feels manageable rather than overwhelming.
One of the most common questions we hear is, “How long will this take?”
The honest answer is: it depends—mostly on the cause, how long the problem has been there, and how consistently we can work on it together.
As a general guideline:
• Mild sprains or strains may improve within a few days to a couple of weeks.
• More significant disc or joint issues often require several weeks to a few months of focused care.
• Long-standing, recurring pain usually takes longer, because the body has adapted to that pattern over time.
In our clinic, we’ll give you a realistic timeline based on your exam and imaging findings. We also schedule progress checks at appropriate intervals so you can see objective changes—not just hope things are better.
The goal is not just quick relief (although we want that too), but a more stable, resilient spine that’s less likely to flare up again.
Most low back pain is mechanical and responds well to conservative care — but there are a few situations where you should seek urgent medical attention instead of (or before) chiropractic care.
Contact your medical doctor or an emergency department immediately if you notice:
Sudden loss of bladder or bowel control
Severe, progressive leg weakness
Numbness in the groin or “saddle” area
A history of cancer with new, unexplained back pain
Unexplained fever, chills, or sudden weight loss with back pain
Significant trauma (like a fall, car accident, or sports injury)
These may be signs of a more serious underlying condition and need prompt medical evaluation.
For most other cases — especially mechanical, posture-related, or recurring low back pain — a thorough chiropractic assessment is an excellent first step.
It’s not always easy to know when low back pain is “just a strain” and when you should get it checked.
It’s a good idea to book a chiropractic assessment if:
• Your low back pain has lasted more than a few days or keeps coming back
• You notice stiffness or soreness most mornings or after sitting
• Pain is starting to interfere with work, exercise, or sleep
• You’re relying more on pain medications just to get through the day
• You’ve tried stretches and self-care but improvements don’t last
A thorough chiropractic assessment can clarify whether your pain is coming from joints, discs, muscles, or a combination—and whether conservative care is appropriate.
For over 20 years, we’ve been helping people in Toronto’s west end move better and feel better—many of them starting with low back pain that had been bothering them for months or even years.
Patients often tell us they appreciate:
• Thorough assessment – We don’t rush; we look at posture, movement, and structure, and use x-rays when indicated.
• Personalized plans – Care is tailored to your specific findings, not a one-size-fits-all protocol.
• Gentle, effective techniques – Adjustments are performed with your comfort and safety in mind, using methods appropriate for your age, build, and condition.
• Integration of home care – We teach simple, realistic exercises and strategies you can actually do at home, so your progress continues between visits.
• Clear communication – You’ll understand what’s happening, what we’re doing about it, and what role you can play in your recovery.
As a trusted Toronto low back pain clinic, we’ve helped thousands of patients find lasting relief through careful assessment, individualized plans, and gentle chiropractic care.
In short, our goal is to help you feel better as quickly as possible, while building a stronger foundation for your spine long term.

Low back pain usually develops from a mix of muscle strain, joint restriction, disc changes, and postural stress. Long hours of sitting, old injuries, and deconditioned core muscles can gradually overload the joints and nerves in your lower back.
You should consider seeing a chiropractor if low back pain keeps returning, lasts more than a few days, or starts limiting your normal activities. A proper assessment can identify whether joints, discs, or muscles are involved and whether conservative care is appropriate for you.
Recovery time depends on the cause of your pain, your general health, and how long the problem has been there. Mild strains may improve within days, while disc or arthritic issues can take weeks to months. Consistent, guided care usually speeds recovery and helps prevent flare-ups.
The most effective treatment often combines gentle spinal adjustments, soft tissue therapy, and simple exercises. Together these approaches restore joint motion, calm irritated muscles and nerves, and help your spine handle everyday stresses again without constant pain.
In many cases, yes. When appropriate, chiropractic care helps reduce pressure on irritated nerves, improve joint motion, and support healing around a disc injury. A careful exam and, if needed, imaging help determine whether conservative chiropractic treatment is suitable for your situation.
Short walks, gentle mobility exercises, and avoiding long stretches of sitting often help. Ice is usually useful early on; heat may help more chronic stiffness. Avoid aggressive stretching or heavy lifting until you’ve been assessed by a spine professional.
Not usually. Most mechanical low back pain can be accurately diagnosed through a detailed history, physical examination, and, when appropriate, digital spinal x-rays.
An MRI is typically reserved for more severe or persistent cases, or when there are neurological red flags that suggest a more serious disc or nerve issue.
In many cases, yes — gentle, controlled movement is more helpful than complete rest.
However, the type of exercise matters. We generally recommend avoiding heavy lifting, high-impact sports, or aggressive stretching until you’ve been assessed.
Once we know what’s going on, we can guide you toward safe movements and gradually reintroduce more activity.
The vast majority of low back pain cases do not require surgery.
Most people improve with conservative treatment that restores joint motion, reduces nerve irritation, and strengthens the supporting muscles.
Surgery is usually considered only when there is severe, unrelenting pain, progressive neurological loss, or when conservative care has been fully tried and hasn’t helped.
Often, yes — but you may need to modify how you work.
We’ll help you understand which positions are safe, how to adjust your workstation or lifting technique, and when to build in short movement breaks to protect your spine while you recover.
Low back pain is common — but it doesn’t have to be a permanent part of your life.
If your pain keeps returning, is lasting longer each time, or is starting to limit your work, sleep, or daily activities, it’s a sign your spine needs more than another stretch or new chair. It needs a clear diagnosis and a structured plan.
At Transform Chiropractic in Toronto, we identify the exact mechanical and structural reasons your back is overloaded and build a personalized plan to help you:
Reduce pain and stiffness
Restore healthy movement
Strengthen and stabilize your spine
Prevent future flare-ups
If you’re ready to stop guessing and start moving in the right direction, we’re here to help.
Book your comprehensive low back assessment today and take the first step toward lasting, natural relief from back pain.
Written by Dr. Byron Mackay, Chiropractor — Transform Chiropractic, Toronto
Last updated November 2025
© 2025 Transform Chiropractic. All Rights Reserved.
Please fill out the form below, including all the required fields, and receive priority new patient scheduling.